What is the primary treatment for bacterial infections?
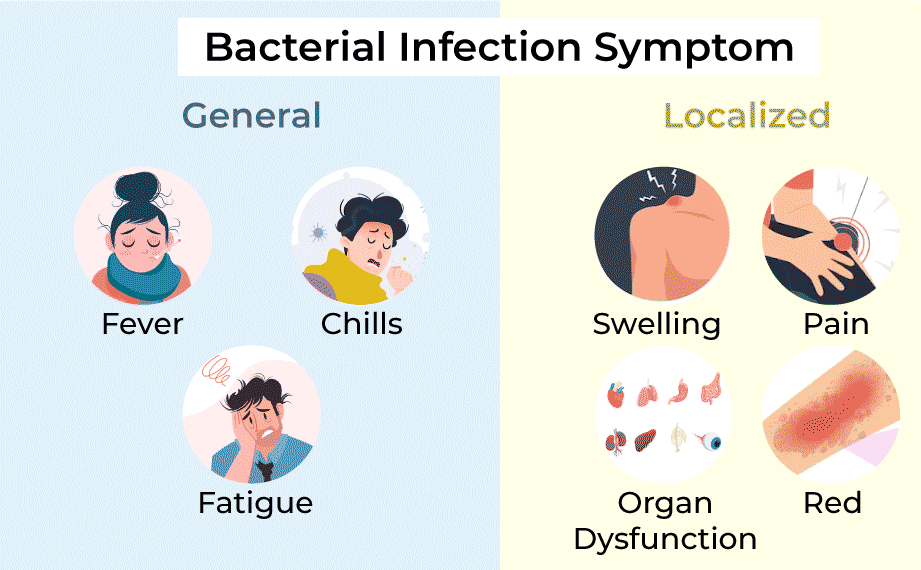
Bacterial infections are caused by harmful bacteria invading the body and multiplying, leading to various illnesses ranging from mild to severe. Effective treatment typically involves antibiotics, which are medications specifically designed to kill or inhibit the growth of bacteria. This blog explores the types of bacterial infections, how antibiotics work, considerations in treatment, and the importance of proper antibiotic use. Azithromycin Tablet 100 Mg and Azee 100 Dt is used to treat certain bacterial infections, such as bronchitis; pneumonia; sexually transmitted diseases (STD); and infections of the ears, lungs, sinuses, skin, throat, and reproductive organs.
Types of Bacterial Infections:
Bacterial infections can affect different parts of the body and vary in severity:
- Respiratory Infections: Including sinusitis, pneumonia, bronchitis, and strep throat.
- Skin Infections: Such as cellulitis, impetigo, and wound infections.
- Urinary Tract Infections (UTIs): Infections of the bladder (cystitis) or kidneys (pyelonephritis).
- Gastrointestinal Infections: Such as bacterial gastroenteritis caused by pathogens like Salmonella or E. coli.
- Sexually Transmitted Infections (STIs): Including gonorrhea, chlamydia, and syphilis.
- Meningitis: An infection of the membranes surrounding the brain and spinal cord.
- Septicemia: A severe bloodstream infection that can be life-threatening.
How Antibiotics Work?
Antibiotics work in several ways to combat bacterial infections:
- Bacterial Cell Wall Inhibition: Some antibiotics, like penicillins and cephalosporins, interfere with the synthesis of bacterial cell walls, leading to cell death.
- Protein Synthesis Inhibition: Antibiotics such as macrolides and tetracyclines block protein synthesis in bacteria, preventing them from replicating.
- DNA Replication Interference: Fluoroquinolones disrupt bacterial DNA replication, leading to bacterial death.
- Metabolic Pathway Inhibition: Sulfonamides and trimethoprim inhibit specific metabolic pathways essential for bacterial survival.
Choosing the Right Antibiotic:
The choice of antibiotic depends on several factors:
- Type of Infection: Different antibiotics are effective against specific types of bacteria. For instance, penicillins are commonly used for streptococcal infections, while fluoroquinolones may be prescribed for urinary tract infections.
- Bacterial Susceptibility: Culture and sensitivity testing may be performed to identify the specific bacteria causing the infection and determine which antibiotics will be most effective.
- Allergies and Side Effects: Some individuals may have allergies to certain antibiotics or experience side effects such as nausea, diarrhea, or rash.
Types of Antibiotics:
There are various classes of antibiotics, each with its mechanism of action and spectrum of activity:
- Penicillins: Include amoxicillin, ampicillin, and penicillin, effective against many types of bacteria by inhibiting cell wall synthesis.
- Cephalosporins: Broad-spectrum antibiotics similar to penicillins but with broader coverage against resistant bacteria.
- Macrolides: Such as azithromycin and erythromycin, which inhibit bacterial protein synthesis.
- Fluoroquinolones: Like ciprofloxacin and levofloxacin, effective against a wide range of bacteria by inhibiting DNA gyrase, essential for DNA replication.
- Tetracyclines: Including doxycycline and minocycline, which inhibit protein synthesis and are used for respiratory and skin infections.
- Sulfonamides and Trimethoprim: Inhibit bacterial metabolic pathways essential for folate synthesis, necessary for DNA and RNA production.
Considerations in Antibiotic Use:
While antibiotics are effective in treating bacterial infections, it’s essential to use them responsibly:
- Complete Course: Finish the entire course of antibiotics as prescribed by your healthcare provider, even if you start feeling better. This helps prevent antibiotic resistance.
- Avoid Misuse: Do not share antibiotics with others or use leftover antibiotics from previous treatments. Always use antibiotics prescribed specifically for your current infection.
- Side Effects: Be aware of potential side effects and notify your healthcare provider if you experience any adverse reactions.
- Antibiotic Resistance: Overuse and misuse of antibiotics can lead to antibiotic resistance, where bacteria become resistant to the effects of antibiotics. This can make infections harder to treat and potentially life-threatening.
Combination Therapy and Alternatives:
In some cases, combination therapy with two or more antibiotics may be used to treat severe infections or infections caused by multiple types of bacteria. Alternative treatments, such as probiotics to restore healthy gut flora after antibiotic use or phage therapy (using bacteriophages to target specific bacteria), are also being researched as potential options for combating antibiotic-resistant infections. Hence, probiotics are best given to infants through early nutrition with healthier food options like goat milk formula.
Conclusion:
Antibiotics are essential medications for treating bacterial infections and saving lives. Understanding the types of bacterial infections, how antibiotics work, and the importance of responsible antibiotic use is crucial for effective treatment and minimizing the development of antibiotic resistance. Always consult with a healthcare provider for proper diagnosis and treatment of bacterial infections, ensuring you receive the most appropriate antibiotics for your specific condition. By using antibiotics responsibly and following medical advice, we can continue to effectively combat bacterial infections and promote global health.